Both for the intensely curious and for my own record-keeping, I thought a few of you may be interested to know what actually happens as you go through this process. As a six-time veteran, I’m probably as much of an “expert” as you’re likely to find…so I’ll share what the experience is like from the patient’s perspective. This will be long and boring for most…but perhaps interesting to a select few!
Both for the intensely curious and for my own record-keeping, I thought a few of you may be interested to know what actually happens as you go through this process. As a six-time veteran, I’m probably as much of an “expert” as you’re likely to find…so I’ll share what the experience is like from the patient’s perspective. This will be long and boring for most…but perhaps interesting to a select few!
1. Pre-Op Consult. The first step in each of these events is a pre-operative consult with the neurosurgeon. At this point, you’re not even sure yet that you’re actually going to have surgery, there’s just something driving the need for a consult…a recurrence, an anomaly on a scan, infection, failed chemo, whatever. In this meeting, you meet with at least one or two nurses who check vitals, ask questions, and perform other tests, and often with at least one other neurosurgeon (resident or attending) before actually meeting with your doctor. Standard neurological exams look for any presentable symptoms — usually targeted to find one-side weakness, blurred vision slurred speech, memory deficits, or other issues. The nurses will give you a long list of instructions about how to proceed prior to surgery, including wonderful details about how and when to eat, shower, and so forth. You have to shower and scrub your scalp with a special soap the night before surgery, and there is no eating or drinking (clear fluids only, if necessary) after midnight the night prior.
With a good exam and strong vitals, you’re off to see the wizard…or, in this case, the head neurosurgeon (Dr. Chu). The neurosurgeon will show you the most recent scan, tell you what he sees and what he thinks, and if there are other opinions from other neurosurgeons or radiologists or oncologists, will likely share those opinions as well. Together, you agree on a plan of treatment — and I truly do mean together. You can decline surgery. The patient’s opinion matters here. You have a say on how aggressive you want to be in attacking the disease. Do you want to try chemo or radiation again before going straight to surgery? Do you want to watch it for a few months to establish a growth pattern? Are you ready to go in now? In the case of this past week, we already knew coming down that it was growing and aggressive, and had already decided on the telephone consult to proceed with surgery, but it was still a good discussion. We agreed to proceed with surgery, which takes us to the next step of…
2. Surgical Clearance. Apparently, brain surgery is a pretty big deal, and takes quite a toll on the body. Because of that, internal medicine and gastroenterology have to do a fair bit of lab work and tests to make sure that your body can withstand not just the surgery, but 8 hours of general anesthesia and all the recovery that goes with it. This normally involves a short EKG (only takes about 10 minutes), another neurological exam, a heart stress test, and for most people a chest x-ray (I got to skip that one). This is all accompanied by many vials of blood that are tested in every way — CBC, Liver Panel, etc — and sometimes urine as well (another one I got to skip). This afternoon of fun can be stressful or problematic if you have any health complications or aren’t in good shape, but for me it’s almost fun to play “stump the doc.” These were the appointments where in prior blogs I was told that they “love my veins” and that I have “an amazing heart.” So after a few hours with Dr. Samadi, I was pronounced healthy enough for surgery, and Dr. Chu’s office was cleared to put me on the schedule. But before venturing into the skull, you have to take a look inside…
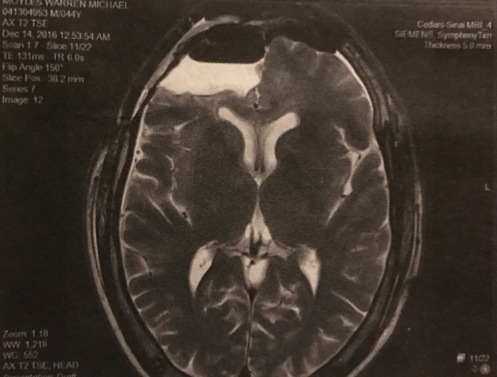
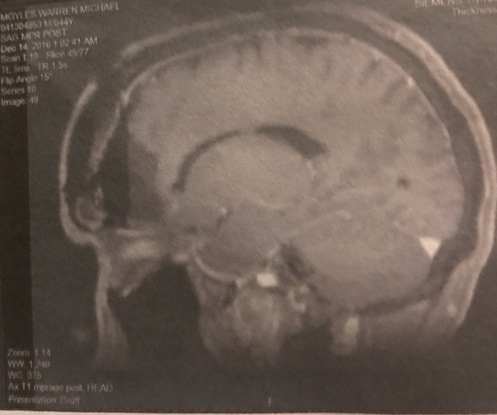
3. Pre-Op MRI. Before making any movement toward surgery, the surgeons need to know what they’re dealing with, and the first step is taking a look inside the brain to see what all the fuss is about. The MRI is just like any other, and for a kid who’s been doing this for 17 years, it’s not much more than a 45-minute nap. However, for many this is still a significant event. It’s loud, uncomfortable, claustrophobic, and generally unpleasant. To reveal malignancies, the neurosurgeon will likely order the MRI “with contrast,” meaning about halfway though the scan, you are pulled out of the machine and given an injection of a chemical called gadolinium, which helps highlight areas in the brain where foreign tissues are active or where the blood-brain barrier has been violated. There are three ways to administer contrast — easy (a shot), hard (an IV), and harder (perfusion). As best I can remember, all of my pre-op scans have been perfusion scans. These scans inject contrast through a large IV (think garden hose), at a very high rate of speed, hoping to expose highlights or enhancements in the brain that other scans may not expose. Better have good, big, strong veins for this one!
If the neurosurgeon suspects that surgery will be necessary, he will order the scan with fiducial markers, which are fancy stickers that are placed on the face and skull during the scan. These stickers show up on the scan, and allow the surgeon to make a firm relationship between the outside and inside of the skull. Not uncomfortable, but a bit intimidating as they draw on you with the purple Sharpie detailing exactly where they want the bone saw to go. By the way, there’s no shower once the fiducials are on…so get that out of the way BEFORE the MRI! With the pre-op consult and scan done, it’s home to get one last meal and try to relax a bit before reporting for surgery the next morning.
4. Surgery Day! I rarely sleep much the night before surgery. The fiducial markers make it difficult, not to mention the nerves and hunger and just mental strain. The morning of surgery, you report to patient admissions two hours prior to your appointed surgery time. Just prior, you shower with the special soap they give you, a disinfectant, taking care not to get your head or any of the fiducial markers wet. Patient admissions is as boring as it sounds…consent forms, paperwork, case history, personal information, and more initials and signatures than you can count. Eventually, you are escorted up to the surgery ward (8th floor) by an orderly, who checks you in at the surgery desk and you wait to be called back. This is one of the most difficult parts for me. I don’t know if I’ll wait five minutes or a few hours, but when your name comes up it’s time to go. No long talks or lengthy goodbyes, you’d better have taken care of those already. A quick hug and kiss to wife and daughter, then a short walk back to the pre-anesthesia care unit. Surrender all your belongings, strip everything, one last bathroom stop, and a thousand more questions and vitals. IV. EKG leads. Meet with the anesthesiologist and neurosurgeon, ensure we are all on the same page, and we are set to go! In my last five surgeries, this is where my memory of events stops. Something special starts dripping into the IV, and the rest is history. But this time, I was still awake when they took me back to…
5. The OR. It is much smaller than I expect. You see these places on television, from ER to General Hospital, and they look huge. It isn’t. About the size of a standard bedroom, with just enough room for the OR table and doctors to move around it. Bright lights, sterile instruments, and someone straps on a mask…”It’s just pure oxygen right now, Mr. Moyles” they lie. “Breathe deeply!”
6. Recovery. Most of the unpleasantness takes place after you’re under general anesthesia. The arterial IV is quite uncomfortable, but allows them to monitor heart rate and blood pressure without a cuff. The catheter is obvoiusly uncomfortable, but is already in place when I wake up. The breathing tube is gone, but the effects of it — a swollen and very sore throat — are some of the most obvious side effects of surgery when waking up. Someone is calling my name, gently shaking my shoulders, and telling me “Wake up, it’s all over.” Slowly, VERY slowly, things begin to materialize, and I’m conscious of the bandages on my head, the people buzzing all around, and a disconcerting number of discomforts…the throat, the dreaded leggings, the IV, the catheter, and numerous other invasions. Once I’m through basic vitals and pupil tests, is pretty much right back to sleep. The pattern of wake/sleep/vitals/sleep continues until I see the most beautiful face in the world (my wife), and beg for my daughter, who appears shortly thereafter. Several more hours, and I skip the Intensive Care Unit (again) and head to a regular patient room.
7. Patent Room. It’s really a glorified hotel room, with LOTS of room service (mostly the undesirable kind). It’s a pretty big room, with areas for visitors and cable TV and a private bathroom. Sounds luxurious to some, but it’s brutal. A first tentative walk, with help, holding an IV pole. Regular visits to check vitals, empty the catheter, update meds and IV fluids, and check drainage, scar/incision, and so forth. Family is there most of the time, and the food is surprisingly good. Occupying the time can be a challenge, but the docs and nurses keep you very busy. Unhooking the IV is a big moment, only to be upstaged by removing the catheter (quite painful). Pain is minimal, and managed well. After about 48 hours after surgery, you’re ready to go home!
Posted in Uncategorized



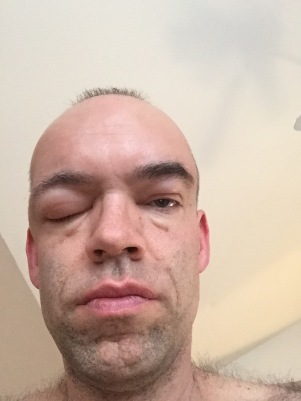
 and labs. He admitted that it wasn’t an infection but that he didn’t know what it was, and couldn’t in good conscience discharge me without knowing what was causing the swelling. He called the on-call neurosurgeon, and after about six hours in the emergency room the neurosurgeon was able to conclude that I had a cerebral spinal fluid leak. This is serious business…untreated, it’s even potentially fatal, or can result in meningitis or hydrocephalus. While going over medical history, I admitted to the doctor that I had not waited the recommended 4 to 6 weeks before strenuous exercise after surgery. In fact, I didn’t even make it two weeks, getting back into my 13 to 15 mile long run routine just 11 days after surgery. It now seems clear that my aggressiveness (exercise addiction? Stubbornness?) likely ruptured some of the internal repairs done after surgery, allowing the cerebrospinal fluid to leak out of the skull and into the open area around the eyes and the sinus. Too far, too fast, too soon…I ignored the doctor’s orders and I definitely paid the price. One slice of that pie, please. Large slice.
and labs. He admitted that it wasn’t an infection but that he didn’t know what it was, and couldn’t in good conscience discharge me without knowing what was causing the swelling. He called the on-call neurosurgeon, and after about six hours in the emergency room the neurosurgeon was able to conclude that I had a cerebral spinal fluid leak. This is serious business…untreated, it’s even potentially fatal, or can result in meningitis or hydrocephalus. While going over medical history, I admitted to the doctor that I had not waited the recommended 4 to 6 weeks before strenuous exercise after surgery. In fact, I didn’t even make it two weeks, getting back into my 13 to 15 mile long run routine just 11 days after surgery. It now seems clear that my aggressiveness (exercise addiction? Stubbornness?) likely ruptured some of the internal repairs done after surgery, allowing the cerebrospinal fluid to leak out of the skull and into the open area around the eyes and the sinus. Too far, too fast, too soon…I ignored the doctor’s orders and I definitely paid the price. One slice of that pie, please. Large slice.